Abstract
This systematic literature review seeks to collate the evidence of the evolution of the role of healthcare information systems (HIS) executive in the United States (US) and to identify the significant events which have influenced the development of this role and its impact on the transformation of healthcare organizations. The HIS executive has evolved over time from the manager responsible for in-house computers, advanced data processing (ADP), communication systems, and system conversions to a participatory member of the executive leadership team responsible for delivering technology solutions which transform the delivery of healthcare. The changes in the responsibilities and the attributes of HIS executives have been driven by changes in technology, standardization of clinical data, government regulation, and the ever-changing reimbursement and business environment. The responsibilities and titles of the HIS executive will evolve and adapt as the business environment and the expectations of consumers and payers change.
Keywords: leadership, delivery of healthcare, health information systems, healthcare outcomes assessment, communication, technology, computers
Introduction
In the US healthcare sector, the role of the healthcare information systems (HIS) executive is recognized as an essential C-suite executive. This position — which typically reports to the chief executive officer (CEO), chief operating officer, or chief financial officer — is generally responsible for harnessing technology to transform the healthcare enterprise in support of organizational objectives such as expansion of healthcare access, improvement in the customer experience, and efficient use of organizational resources. Although the HIS executive has responsibility for the strategy and direction of the technology resources and functions, the day-to-day management of these resources resides with other managers who report to this executive. While today, the HIS executive is a prominent member of the executive team and often responsible for digital transformation, this has not always been the case and may not be the case in the future.
Early History of HISs
The American Hospital Association and the Healthcare Information and Management Systems Society began educating hospital administrators about the potential of HIS in the 1950s.1-3 By the late 1950s, researchers were studying the models employed by physicians for clinical decision making with the intent to develop HISs4-8 to improve the quality of patient care, increase the legibility and accessibility of medical records, and enable rapid communication of data for clinical care.9, 10
Although hospitals were employing computers in the 1960s for business, accounting, medical research,11 and limited patient care applications,12 no firm had a working HIS.13 Meaningful advances toward a HIS were limited by technology, cost, programming languages under development, and the supply of qualified personnel.14 Few computer applications were available to aid in the delivery of patient care and the available programs could not easily be adapted for use by other organizations.11, 15 Specialized knowledge of computer syntax was required to use HISs and the number of users who could interact with the system simultaneously was limited.16, 15
The Heart, Cancer and Stroke Act17 established the National Advisory Council on Regional Medical Programs18 which funded 54 Regional Medical Programs (RMPs), and in part, underwrote development of clinical laboratory systems, clinical data collection systems, multiphasic screening systems, and tumor registries.19 The passage of the Heart Disease, Cancer, Stroke, and Kidney Disease Amendments20 reauthorized the RMPs and supported continued development of HISs at Kaiser Permanente,21-27 the Harvard Community Health Plan,28, 29 LDS Hospital,30, 31 and other academic medical centers.
The first successful commercial HIS, the TDS Healthcare Systems Corporation’s Health Care 4000 System, began development in 1964, installation in 1971, and was fully accepted in 1974.32-35 By 1980, there were eighteen vendors of first-generation Level 1 HISs and six vendors of second-generation Level 1 HISs.36, 37 Even though many healthcare and commercial organizations developed HISs, these systems were described as “…obsolete, fragmented, and poorly conceived”,38 “…blunt testimony to the difficulties of implementing computer-based information systems for health care delivery”,39 as well as “…designed to collect and aggregate data rather than to serve as decision support systems”.40 Testimony before Congress suggested that commercial development of comprehensive HISs was not financially feasible; that changes in reimbursement by government insurance programs had limited investment; and, that studies did not exist which demonstrated cost savings could be achieved through implementation of HISs.41, 42
With passage of the Tax Equity and Fiscal Responsibility Act (TEFRA),43 Medicare transitioned reimbursement of hospitals to a prospective payment system (PPS).44 PPS required HISs capable of providing information for each department, service, or unit, and linking this data to the medical record and hospital bill.45-48 Inaccurate reporting of data led to underpayment of hospitals49 and resulted in approximately half of all hospitalized patients being treated at a loss and the financial failure of hospitals.50 The information processing requirements and the complexity of PPS led to the appointment of HIS executives to manage the strategy and direction of HISs.
Objective
The first study, which attempted to define the primary attributes of the chief information officer (CIO), was undertaken by the Society of Management Information Systems in 1982.51 Further research to identify the evolving role of the CIO were conducted in economic sectors such as banking, retail, manufacturing, automotive, and transportation;52-54 however, there are limited studies which include healthcare organizations and no studies which specifically explore the topic from the healthcare perspective. The objective of this systematic review is to collate the evidence of the growth of the role of the HIS executive in the US as well as to identify significant events which influenced the evolution of the role.
Methods
Eligibility Criteria, Information Sources, and Search Strategy
Documents eligible for this review included literature published in English and which provides evidence of the role of the HIS executive. As computer usage in hospitals did not begin until the 1960s11 and the title chief information officer or the acronym CIO were not introduced until 198055 and 197956 respectively, no documents prior to the 1960s were expected to be identified. As the objective of the study was to collate evidence of the evolution of the role in healthcare, literature was not limited to a specific healthcare setting.
Seven databases were searched to identify documents: Academic Search Premier, Scopus, Business Search Premier, ABI/Inform, PubMed, CINAHL, and Ovid MEDLINE. The list of periodicals and other publications searched by each database were reviewed to ensure appropriate coverage of the business and healthcare literature. The search strategy included three main topics: healthcare or medical delivery, information systems management or leadership, and role. To identify the relevant documents, key words and index terms were used in conjunction with Boolean operators customized to the search engine of each database.
Figure 1 illustrates the search process which was undertaken. Documents identified by the database searches were initially screened by title, keywords, and abstract. Documents meeting criteria were identified and full text documents obtained and reviewed. The snowball method was used to identify additional documents. EndNote 2157 was used to manage the documents.
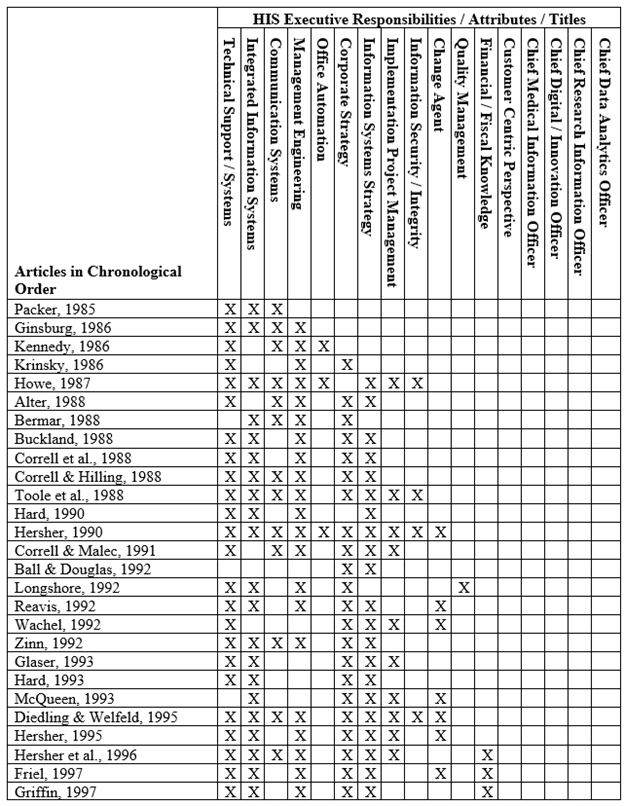
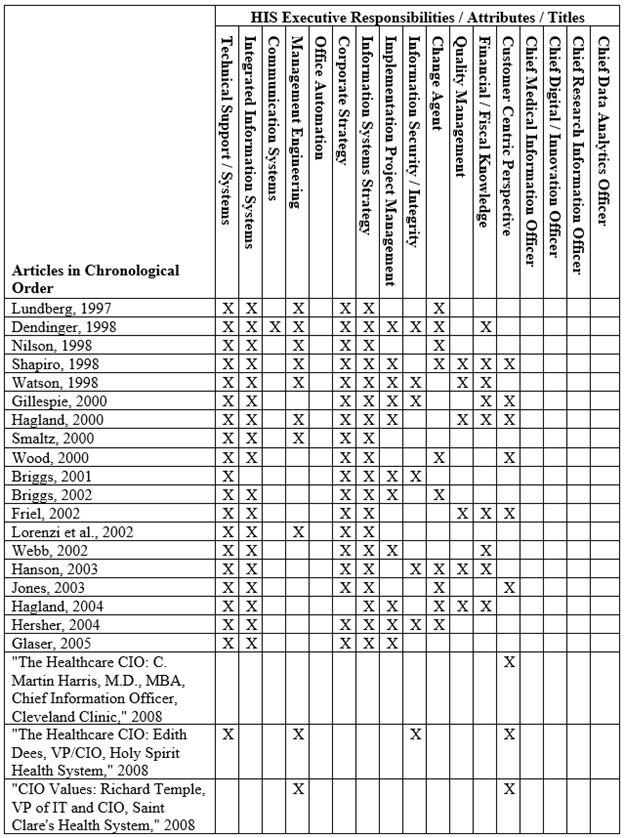
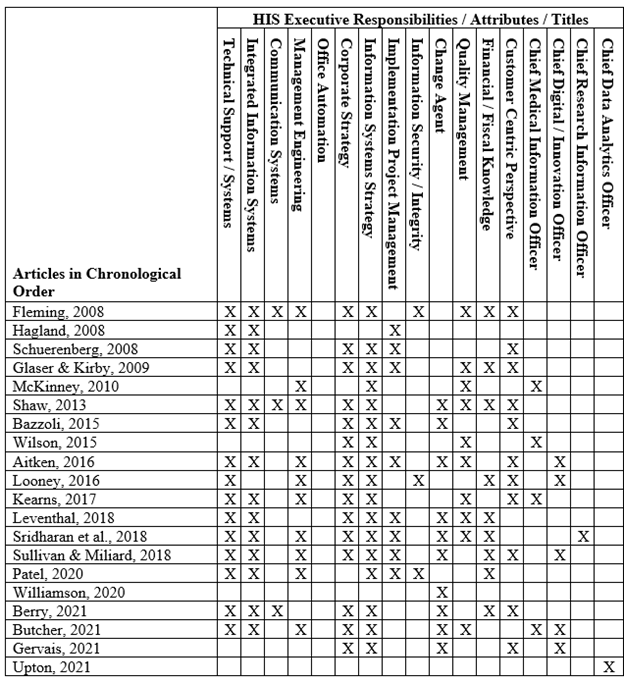
The initial search of the seven databases yielded 166 documents of which ten were duplicates. Review of titles, keywords, and abstracts resulted in 100 documents being eliminated. One document from a trade journal by an anonymous author could not be obtained. The snowball method identified 64 additional documents. A total of 69 documents were included in this study. The documents were analyzed using an inductive approach to identify implicit and explicit titles, responsibilities, and attributes which are presented in chronological order in Table 1.
Results
Of the 69 documents that met inclusion criteria, one document was a book, five documents were book chapters, nine documents appeared in scholarly journals, 51 documents appeared in trade periodicals, and three were electronic articles. The first document was published in 1985 and the last in 2021. Of the documents published in scholarly journals, three were interviews with industry incumbents, two were columns by industry incumbents, one was an editorial, one discussed the results of an industry survey, one discussed the results of a survey conducted by the author, and one was a review. All documents discussed the titles, responsibilities, and / or attributes of HIS executives with 52 documents detailing the role in hospitals or health systems, ten in the general healthcare sector, four in the pharmaceutical setting, one in the behavioral health setting, one in life sciences setting, and one in the managed care setting.
The Rise of the HIS Executive
In the 1960s, hospital administrators were challenged to lead the development of HISs with the assistance of a “master craftsman” in advanced data processing (ADP).58 Even though technology evolved during the 1970s and 1980s, the HIS executive continued to be viewed as a technician responsible for in-house computers, ADP, and system conversions rather than a participatory member of the executive team.59 As multi-hospital systems emerged, purchases and implementation of computer hardware and software were centralized60 and the role of the HIS executive was recognized in theory but not in practice.61 Healthcare’s reliance upon computers increased as the requirements for financial, patient, and employee data grew and led to increased recruitment of “healthcare’s rare bird”,62 the CIO. Further, the industry struggled with the title of the HIS executive63 although the most common title was vice president of information systems.64, 65 Even though organizations recognized the need to move to patient oriented rather than financial oriented information systems,66 there was no consensus on the individual responsible, their title, their qualifications, and even the need for a senior executive to manage HIS.67-69
The enactment of TEFRA and the introduction of PPS increased healthcare organizations’ focus on information management, HISs, and the individuals responsible for these systems. By the late 1980s, HIS executives recognized one of their major responsibilities as strategic planning although fewer than half of all hospitals had a plan for information systems.70 Among the first healthcare organizations to recognize the need to focus information systems on business rather than technical requirements was American Medical International with the appointment of their first CIO in 1987.71 Many healthcare organizations struggled with the type and source of required information as well as the qualifications of the executive responsible for managing this resource.69 From 1988 to 1990, the number of hospitals with CIOs increased by 500 percent with approximately ten to fifteen percent of hospitals having a CIO.72 However, the development of HISs was limited due to lack of clinical terminology standards,73-77 effective physician interface,78, 79 lack of standards from professional organizations,80, 77, 81, 73, 82 and lack of government funding for replacement of the paper-based medical record.83, 73
The 1990s saw the passage of the Health Insurance Portability and Accountability Act (HIPAA),84 the Balance Budget Act (BBA),85 and preparation for the year 2000 (Y2K) which influenced organizations’ investments in HISs. The enactment of HIPAA imposed new standards for information privacy and security with a projected five year cost of $22.5 billion for the industry to reconfigure or replace information systems86 and an overall cost of $43 billion.87-91 The BBA was projected to reduce hospital payments by $53 billion over five years however actual reductions reached $71 billion92 and curtailed HIS investment. Preparation for Y2K saw healthcare organizations seeking HIS executives with strong technical skills to lead their organizations through this crisis.93 In response to Y2K, organizations devoted an estimated $8.5 billion of capital and other resources to assess, update, and replace equipment93-97, 90 and, at least in the short-term, halt or postpone HIS strategic initiatives98, 97 as well as consider outsourcing as a solution to relieve recruitment challenges and the short-term need for capital.93, 99
In the 1990s organizations began to recognize that HIS executives were no longer technicians who oversaw hardware and software, integrated systems to support their organizations, ensured data integrity and security, and were responsible for implementation and project management but were now members of the senior management team who provided a strategic vision for the HIS platform,100-102, 72, 103-109, 94, 110-115 aligned corporate and HIS strategies, 100, 103, 101, 116, 102, 104-106, 117, 107, 108, 112, 113, 118, 109, 114, 94, 110, 115, 111 functioned as agents of change,102, 104, 100, 107, 108, 94, 110, 112, 119, 114, 115 and provided insight into the potential financial impact of HISs on the healthcare enterprise.109, 94, 111, 115 Although organizations recognized the need for HIS executives to possess these skills, CEOs felt HIS executives lacked a strategic and operational orientation as well as failed to understand the industry.120
Even though Congress assigned responsibility to the Agency for Health Care Policy and Research for developing automated medical record standards121 the agency chose to rely upon private entities to develop the standards.73 The 2000s saw the formation of a public private partnership composed of healthcare organizations, payers, accreditors, government agencies, researchers, and HIS suppliers to facilitate the development and adoption of national clinical data standards.122 The Medicare Prescription Drug, Improvement, and Modernization Act123 was passed and created interoperability standards and incentives for adoption of e-prescribing.124 The executive branch established the Office of the National Coordinator for Health Information Technology (ONC) and the position of the National Health Information Technology Coordinator to create incentives for the use of health information technology.125 The Certification Commission for Health Information Technology was formed at the request of the ONC to design, develop, and implement testing and cerfication of electronic health record products.126, 127 Based upon the recommendations made in The ONC-Coordinated Federal Health IT Strategic Plan: 2008-2012128 the Health Information Technology for Economic and Clinical Health Act (HITECH)129 was passed and created incentives, at least initially, for the adoption of HISs.
The role of the HIS executive continued to evolve during the 2000s. In addition to the skills developed in the 1980s and 1990s, HIS executives were required to develop a more customer centric focus by ensuring internal and external customer satisfaction;130, 131 developing a consumer oriented skill set;132, 133 selling the benefits of technology to stakeholders;134 empowering consumers to take charge of their healthcare;135, 136, 131, 133 delivering projects on time, on budget, and with expected benefits;137 being able to communicate with employees at all levels of the organization;138 and to engaging executives, clinicians, staff, and patients in development of HISs.139, 136, 131
In 2010, the Patient Protection and Affordable Care Act,140 and its amendments in the Health Care Education Reconciliation Act,141 generally referred to as the Affordable Care Act (ACA), were signed into law. While the ACA did not contain specific provisions for adoption of HISs, many initiatives such as testing of new delivery models, paying for value rather volume, and adopting innovations from the Center for Medicare and Medicaid Innovation and the Patient-Centered Outcomes Research Institute, or measuring progress toward achievement of the goals of the National Strategy for Quality Improvement in Health Care required the use of HISs. In 2011, CMS established the Medicare and Medicaid Electronic Health Record (EHR) Incentive Program to encourage eligible professionals and hospitals to adopt a certified EHR and demonstrate meaningful use142 through data capture and sharing, electronic data exchange for advanced clinical processes, and demonstration of improved outcomes.143
The 2010s saw several new titles for HIS executives. The chief medical information officer (CMIO), sometimes known as the chief clinical information officer, was initially hired to facilitate physician use of HISs as organizations deployed or modified EHRs to meet the requirements of the incentive programs.144, 145 CMIOs were involved in decision making and coordinating clinical goals with information technology strategies146 and evolved to take on a more strategic role by assisting organizations with gaining value from their investments in HISs.144, 147 The chief research information officer (CRIO) emerged in academic healthcare organizations where the CRIO oversaw the coordination of information systems which supported research activities.148 The chief digital officer (CDO) or chief innovation officer (CINO) entered the HIS executive ranks with a focus on the external environment and identifying new ways to interact with customers while the CIO remained focused on internal strategies, operations, and delivering digital transformation.149-151 To some, the CDO is a stop gap position which will no longer exist as digital health becomes another channel of healthcare delivery.151
On January 31, 2020, the Secretary of the HHS declared a public health emergency152 after the CDC determined that COVID-19 could be spread from human-to-human.153 Congress responded by passing the Coronavirus Aid, Relief, and Economic Security Act which authorized the Health Resources and Services Administration to provide grants for telemedicine infrastructure and equipment and Medicare to waive telehealth restrictions and encourage expansion of telehealth services.154
COVID-19 required healthcare organizations to develop innovative ways to onboard and train new employees and medical staff members155 as well as rapidly transition patient care and the patient experience to the digital environment.156 HIS executives played a crucial role by rapidly expanding telehealth capabilities, implementing business analytics and mobile technologies to track organizational resources and communicate clinical data, and ensuring HIS infrastructure was secure from cyber-attacks.157 Healthcare organizations continued to struggle with the titles given to HIS executives158 with the chief data officer, chief data and analytics officer, chief data and AI officer, chief information security and data officer, and the chief data strategist and solutions officer joining the ranks of the HIS executives.159
Discussion
The role of the HIS executive has evolved over time from the manager responsible for HISs and other technical systems to a participatory member of the executive team responsible for delivering technology solutions which transform the delivery of healthcare. As demonstrated in Table 1, not only have the responsibilities of the individuals changed but also their backgrounds, titles, and attributes. The HIS executive has evolved from a technician to a business leader and now includes individuals with clinical backgrounds who understand clinical workflows and outcome measures. The changes in the responsibilities given to and the attributes expected of HIS executives have been driven by changes in technology, standardization of clinical data, government regulation, the ever-changing reimbursement and business environment, as well as the changing expectations of payers and consumers.
Limitations and Future Research
Several limitations are inherent in the study. During the screening and selection processes, selection bias is a concern. The search syntax employed attempted to capture the largest number of relevant documents but may not have captured all. Publication bias exists as the initial search was limited to research databases and these databases restrict the publications searched, the years searched, and only capture published documents. To mitigate this limitation, the searches were not limited to peer reviewed articles but also included books, book chapters, industry publications, newspapers, news wire releases, and gray literature. Finally, restraining the dates searched may also limit the relevant information identified. The search syntax employed did not restrain the searches to a specific date range and selection of the databases ensured appropriate coverage of the business and healthcare literature from 1946 forward. However, the searches were conducted in May 2023, so no documents published or added to the databases after this date were identified in the study.
As the subject of this study is not well covered in the academic literature, future research should seek to understand the changing role of the HIS executive and the factors which are influencing the changes in the titles, responsibilities, the attributes of the incumbents, as well as the expectations of the individuals to whom HIS executives report. Further, although academic literature is limited, documents discussing the role in the hospital or health system setting are available while documents exploring this role in other healthcare sectors are limited. This suggests future research should seek to understand the expectations and the influence of the external environment within each sector, as well as commonalities which may exist across the sectors. Finally, the findings suggest academic programs must understand the influence of the external and internal environments and the skills expected of individuals entering this field and develop curricula and programs aimed at growing future HIS leaders.
The Scottsdale Institute provided financial support for the project and there are no other conflicts of interest to disclose.
Conclusions
The role of the HIS executive will continue to evolve as technology, regulation, and the business environment change. The responsibilities given to the HIS executive will shift as the expectations of consumers and payers evolve. Digital health will become another channel of healthcare delivery with the expectation that all leaders, not just HIS leaders, be able to convert data into actionable strategies which transform their organizations.
References
1. Collen, Morris F. The History of Medical Informatics in the United States. 2nd ed. Edited by Marion J Ball. London, UK: Springer, 2015. doi:10.1007/978-1-4471-6732- 7_6.
2. HIMSS Legacy Workgroup. History of the Healthcare Information and Management Systems Society: 1961-2006. Chicago, IL: Healthcare Information and Management Systems Society (HIMSS), 2007.
3. Jydstrup, Ronald A, and Malvern J Gross. "Cost of Information Handling in Hospitals." Health services research 1, no. 3 (Winter 1966): 235-271.
4. Ledley, Robert S, and Lee B Lusted. "Reasoning Foundations of Medical Diagnosis; Symbolic Logic, Probability, and Value Theory Aid Our Understanding of How Physicians Reason." Science 130, no. 3366 (1959): 9-21. https://doi.org/10.1126/science.130.3366.9.
5. Warner, Homer R, Alan F Toronto, L George Veasey, and Robert Stephenson. "A Mathematical Approach to Medical Diagnosis: Application to Congenital Heart Disease." Journal of the American Medical Association 177, no. 3 (1961): 177-183. https://doi.org/10.1001/jama.1961.03040290005002.
6. Scheff, Thomas J. "Decision Rules, Types of Error, and Their Consequences in Medical Diagnosis." Behavioral Science 8, no. 2 (1963): 97-107.
7. Collen, Morris F, Leonard Rubin, Jerzy Neyman, George B Dantzig, Robert M Baer, and A B Siegelaub. "Automated Multiphasic Screening and Diagnosis." American journal of public health and the nation's health 54, no. 5 (May 1964): 741-750. https://doi.org/10.2105/AJPH.54.5.741.
8. Scadding, John Guyett. "Diagnosis: The Clinician and the Computer." The Lancet 290, no. 7521 (Oct 21 1967): 877-882. https://doi.org/10.1016/S0140-6736(67)92608-6.
9. Yoder, Richard D. "Preparing Medical Record Data for Computer Processing." Hospitals 40 (Aug 16 1966): 75-76, 83-85.
10. Brenner, M Harvey, and E Richard Weinerman. "An Ambulatory Service Data System." American journal of public health and the nation's health 59, no. 7 (Jul 1969): 1154-1168. https://doi.org/10.2105/AJPH.59.7.1154.
11. McCarn, David B, and David G Moriarty. "Computers in Medicine." Hospitals 45 (Jan 1 1971): 37-39.
12. Barnett, G Octo. "Computers in Patient Care." New England Journal of Medicine 279, no. 24 (Dec 1968): 1321-1327.
13. Siler, William, and Henry Korn. "A Working Total Information System Is at Least a Year Away." Hospitals 41 (May 1 1967): 99-104.
14. Hoffman, Paul B, and G Octo Barnett. "Time-Sharing Increases Benefits of Computer Use." Hospitals 42 (Jun 16 1968): 62-67.
15. Gardner, Reed M. "The Place of Computers in Medicine." Computer 8, no. 1 (1975): 18-19. https://doi.org/10.1109/C-M.1975.218748.
16. Kiely, Joseph M, John L Juergens, Bradner L Hisey, and Paul E Williams. "A Computer-Based Medical Record: Entry of Data from the History and Physical Examination by the Physician." Journal of the American Medical Association 205, no. 8 (1968): 571-576. https://doi.org/10.1001/jama.1968.03140340041010.
17. Heart Disease, Cancer, and Stroke Amendments of 1965. Pub. L. No. 89-239, 900 et seq, 682 Stat. 1965.
18. Huntley, Robert R. "Programs of the National Center for Health Services Research and Development: Evaluation Research." Medical Care 7, no. 2 (Mar-Apr 1969): 86-91.
19. Collen, Morris F. "Origins of Medical Informatics." Western Journal of Medicine 145, no. 6 (Dec 1986): 778-785.
20. Heart Disease, Cancer, Stroke, and Kidney Disease Amendments of 1970. Pub. L. No. 91-515, 101 et seq, 299 Stat. 1970.
21. Van Brunt, Edmund E, Morris F Collen, Lou S Davis, E Besag, and Samuel J Singer. "A Pilot Data System for a Medical Center." Proceedings of the Institute of Electrical and Electronics Engineers 57, no. 11 (Nov 1969): 1934-1940. https://doi.org/10.1109/PROC.1969.7439.
22. Davis, Lou S. "Prototype for Future Computer Medical Records." Computers and biomedical research 3, no. 5 (1970): 539-554. https://doi.org/10.1016/0010-4809(70)90015-7.
23. Collen, Morris F. "Development of Health Systems II." Paper presented at the International Conference on Future Goals of Engineering in Biology and Medicine, Washington, DC, Sep 1967.
24. Collen, Morris F. "The Multitest Laboratory in Health Care of the Future." Hospitals 41, no. 9 (May 1967): 119-125.
25. Davis, Lou S, Morris F Collen, Leonard Rubin, and Edmund E Van Brunt. "Computer-Stored Medical Record." Computers and biomedical research 1, no. 5 (May 1968): 452-469.
26. Garfield, Sidney R. "The Delivery of Medical Care." Scientific American 222, no. 4 (Apr 1970): 15-23.
27. Collen, Morris F, and Lou S Davis. "Computerized Medical Records in Multiphasic Testing." Computer 6, no. 7 (Jul 1973): 23-28. https://doi.org/10.1109/MC.1973.6535358.
28. Barnett, G Octo. "The Application of Computer-Based Medical-Record Systems in Ambulatory Practice.". New England Journal of Medicine 310, no. 25 (Jun 21 1984): 1643-1650. https://doi.org/10.1056/nejm198406213102506.
29. Barnett, G Octo, Norma S. Justice, Michael E Somand, J Barclay Adams, Bruce D Waxman, Peter D Beaman, Monica S Parent, Fredric R Van Deusen, and Jacqueline K Greenlie. "Costar-a Computer-Based Medical Information System for Ambulatory Care." Proceedings of the IEEE 67, no. 9 (Sep 1979): 1226-1237. https://doi.org/10.1109/PROC.1979.11438.
30. Warner, Homer R., Charles M Olmsted, and Barry D Rutherford. "HELP—a Program for Medical Decision-Making." Computers and biomedical research 5, no. 1 (1972): 65-74. https://doi.org/10.1016/0010-4809(72)90007-9.
31. Pryor, T Allan, R M Gardner, P D Clayton, and Homer R Warner. "The HELP System." Paper presented at the The Sixth Annual Symposium on Computer Applications in Medical Care, Oct 30 - Nov 2 1982.
32. Hodge, Melville H. Medical Information Systems: A Resource for Hospitals. Germantown, MD: Aspen Systems Corp., 1977.
33. Plotnick, Rachel. "Computers, Systems Theory, and the Making of a Wired Hospital: A History of Technicon Medical Information System, 1964-1987." Journal of the American Society for Information Science and Technology 61, no. 6 (2010): 1281-1294. https://doi.org/10.1002/asi.21324.
34. Stead, William W, and W Edward Hammond. "Computer-Based Medical Records: The Need for Storing a Single Datum in Multiple Orientations." Paper presented at the The Twelfth Annual Symposium on Computer Applications in Medical Care, Washington, DC, Nov 6-9 1988.
35. Stead, William W, and W Edward Hammond. "Computer-Based Medical Records: The Centerpiece of TMR.". MD Computing 5, no. 5 (Sep-Oct 1988): 48-62.
36. Ball, Marion J, and Stanley E Jacobs. "Hospital Information Systems as We Enter the Decade of the 80's." Paper presented at the The Fourth Annual Symposium on Computer Applications in Medical Care, Washington, DC, Nov 2-5 1980.
37. Ball, Marion J, and Stanley E Jacobs. "Information Systems: The Status of Level 1." Hospitals 54 (1980): 179.
38. Connors, Edward J. "Hospital System Aspects." Chap. 2 In Operations Research in Health Care: A Critical Analysis, edited by Larry J Shuman, R Dixon Speas and John P Young, 29. Baltimore, MD: The Johns Hopkins University Press, 1975.
39. Giebink, Gerald A, and Leonard L Hurst. Computer Projects in Health Care. xii. Ann Arbor, MI: Health Administration Press, Sep 20, 1975.
40. Austin, Charles J, and Barry R Greene. "Hospital Information Systems: A Current Perspective." Inquiry 15, no. 2 (1978): 106.
41. Congress of the United States. Use of Information Technology in Hospitals. Statement of Melroy D. Quasney, Associate Director, Information Management and Technology Division, Hearings before the Subcommitte on Education and Health. 100th Congress of the United States. 853-868 (1988).
42. Glandon, Gerald L., and Roberta J. Shapiro. "Benefit-Cost Analysis of Hospital Information Systems: The State of the (Non) Art." Journal of Health and Human Resources Administration 11, no. 1 (Summer 1988): 30-92.
43. Tax Equity and Responsibility Act of 1982. Pub. L. No. 97-248, 101 et seq, 234 Stat. 1982.
44. Barnard, Cynthia. "Preparing for Case Mix: The Role of Data Processing." Healthcare Financial Management 37, no. 6 (Jun 1983): 57-70.
45. Rogerson, Charles L. "Towards a Case-Mix Information System for the Emergency Department." Paper presented at the The Eighth Annual Symposium on Computer Application in Medical Care, Washington, DC, Nov 4-7 1984.
46. Vladeck, Bruce C. "Medicare Hospital Payment by Diagnosis-Related Groups." Annals of internal medicine 100, no. 4 (1984): 576-591.
47. Dobson, Allen. "The Medicare Prospective Payment System: Intent and Future Direction." Paper presented at the Annual Symposium on Computer Application in Medical Care, 1984.
48. Bassett, J G. "Cost-Per-Case Reimbursement: A Challenge to Hospital Management." Topics in Health Record Management 4, no. 3 (Mar 1984): 1-9.
49. Ertel, Paul Y. "Accuracy in the Reporting of Clinical Data: Proper Roles for the Physician and the Computer." Paper presented at the The Eighth Annual Symposium on Computer Application in Medical Care, Washington, DC, Nov 4-7 1984.
50. Flanagan, Patrick. "Emergency Treatment for Health Care Systems.". Computer Decisions 20, no. 9 (Sep 1988): 43.
51. Rockart, John F., Leslie Ball, and Christine V. Bullen. "Future Role of the Information Systems Executive." MIS quarterly 6, no. Special Issue (Dec 2 1982): 1-14. https://doi.org/10.2307/248989.
52. Feeny, David F, and Leslie P Willcocks. "Core Is Capabilities for Exploiting Information Technology." MIT Sloan management review 39, no. 3 (Spring 1998): 9.
53. Chun, Mark, and John Mooney. "CIO Roles and Responsibilities: Twenty-Five Years of Evolution and Change." Information & management 46, no. 6 (2009): 323-334.
54. Peppard, Joe, Chris Edwards, and Rob Lambert. "Clarifying the Ambiguous Role of the CIO." MIS Quarterly Executive 10, no. 1 (2011): 31-44.
55. Winkler, Connie. "Manager Must Be Superman, Conferees Told.". Computerworld 14, no. 43 (Oct 20 1980): 20.
56. Synnott, William R. "Strategic Planning for Information Management Effectiveness.". Infosystems 26, no. 10 (Oct 1979): 70.
57. Endnote Version 21.2. Clarivate Analytics LLC, Philadelphia, PA.
58. Jacobus, Gilbert C. "Sorting Sense from Nonsense in Hospital ADP Programs." Hospitals 41 (May 1 1967): 32-36.
59. Packer, C L. "The CIO: An Emerging Hospital Executive." Hospitals 59, no. 16 (Aug 16 1985): 144-149.
60. Ginsburg, Debra A. "Changes in the Healthcare Information Systems Marketplace: The Role of Chief Information Officer." Healthcare Computing & Communications 3, no. 12 (Dec 1986): 66-68.
61. Kennedy, O George. "Is There a Need for a Chief Information Officer?". Healthcare Financial Management 40, no. 2 (Nov 1986): 106.
62. Krinsky, Mark L. "The Chief Information Officer -- Capturing Healthcare's Rare Bird." Computers in Healthcare 7, no. 8 (Aug 1986): 66.
63. Howe, Richard C. "CIO, VP MIS, MIS Director, DP Manager--Who Cares?". Healthcare Computing & Communications 4, no. 9 (Sep 1987): 44-45.
64. Bermar, Amy. "Role of CIO Eludes Hospitals' Top Info Execs." PC Week 5, no. 18 (May 3 1988): C6.
65. Correll, Richard A, and Levi N Hilling. "Healthcare CIOs-National Survey Results." Journal of the Healthcare Information and Management Systems Society 2, no. 2 (Summer 1988): 6-7.
66. Korpman, Ralph A. "Using the Computer to Optimize Human Performance in Health Care Delivery. The Pathologist as Medical Information Specialist.". Archives of Pathology & Laboratory Medicine 111, no. 7 (Jul 1987): 637-645.
67. Toole, Jay E, Lee Cort, and Richard A Correll. "Is There a CIO in Your Future." Healthcare Executive 3, no. 1 (Jan/Feb 1988): 30-33.
68. Correll, Richard A, Wendell Finkbeiner, Levi N Hilling, David M McConkey, G Malcom Murray, and Jay E Toole. "Information Management: Emergence of a New Deal. Roundtable on Information Management.". Healthcare Financial Management 42, no. 6 (Jun 1988): 23-24, 28-30, 36-38.
69. Buckland, Ann E. "Chief Information Officer--Try It on for Size." Journal of the American Medical Record Association 59, no. 8 (Aug 1988): 34-39.
70. Alter, Allan E. "Intensive Care.". CIO 1, no. 7 (Jun 1988): 22.
71. Weixel, Suzanne. "CIO Writes MIS Rx.". Computerworld 22, no. 3 (Jan 18 1988): 68.
72. Hard, Rob. "CEOs Take a New Look at the CIO Function." Hospitals 64, no. 11 (Jun 5 1990): 64.
73. United States General Accounting Office. Automated Medical Records: Leadership Needed to Expedite Standards Development. Washington, DC, 1993.
74. Evans, David A, James J Cimino, William R Hersh, Stanley M Huff, Douglas S Bell, and Canon Group. "Toward a Medical-Concept Representation Language." Journal of the American Medical Informatics Association 1, no. 3 (May/Jun 1994): 207-217.
75. Cimino, James J. "Coding Systems in Health Care." Yearbook of Medical Informatics 4, no. 1 (1995): 71-85. https://doi.org/10.1055/s-0038-1638022.
76. White, Kerr L. "Restructuring the International Classification of Diseases: Need for a New Paradigm." Journal of Family Practice 21, no. 1 (Jul 1985): 17-20.
77. Cimino, Christopher, and G Octo Barnett. "Standardizing Access to Computer-Based Medical Resources." Paper presented at the Fourteenth Annual Symposium on Computer Application in Medical Care, Washington, DC, Nov 4-7 1990.
78. Nowlan, W A, A L Rector, S Kay, C A Goble, B Horan, T J Howkins, and A Wilson. "Pen & Pad: A Doctors' Workstation with Intelligent Data Entry and Summaries." Paper presented at the Fourteenth Annual Symposium on Computer Application in Medical Care, Washington, DC, Nov 4-7 1990.
79. Silva, John S, Anthony J Zawilski, John O'Brian, Neal Gunby, Jason Siegel, Mark Lauteren, and Robin Halley. "The Physician Workstation: An Intelligent “Front End” to a Hospital Information System." Paper presented at the Fourteenth Annual Symposium on Computer Applications in Medical Care, Washington, DC, Nov 4-7 1990.
80. McDonald, Clement J, and William E Hammond. "Standard Formats for Electronic Transfer of Clinical Data." Annals of internal medicine 110, no. 5 (Mar 1989): 333-335.
81. Harrington, John J, Timothy J R Benson, and Andrew L Spector. "IEEE P1157 Medical Data Interchange (MEDIX) Committee Overview and Status Report." Paper presented at the Fourteenth Annual Symposium on Computer Applications in Medical Care, Washington, DC, Nov 4-7 1990.
82. Shabot, M Michael. "Standardized Acquisition of Bedside Data: The IEEE P1073 Medical Information Bus." International Journal of Clinical Monitoring and Computing 6 (Dec 1989): 197-204. https://doi.org/10.1007/BF01733623.
83. Barnett, G Octo, Robert A. Jenders, and Henry C Chueh. "The Computer-Based Clinical Record - Where Do We Stand?". Annals of internal medicine 119, no. 10 (Nov 15 1993): 1046-1048. https://doi.org/10.7326/0003-4819-119-10-199311150-00014.
84. Health Insurance Portability and Accountability Act of 1996. Pub. L. No. 104-191, 201 et seq, 110 Stat. 1996.
85. Balance Budget Act of 1997. Pub. L. No. 105-33, 1001 et seq, 251 Stat. 1997.
86. First Consulting Group. The Impact of the Proposed HIPAA Privacy Rule on the Hospital Industry. American Hospital Association, (Chicago, IL: American Hospital Association, Dec 2000).
87. Eddy, A Craig. "A Critical Analysis of Health and Human Services' Proposed Health Privacy Regulations in Light of the Health Insurance Privacy and Accountability Act of 1996." Annals of health law 9 (2000): 1-72.
88. Tieman, Jeff. "One Huge HIPAA." Modern Healthcare 30, no. 52 (Dec 18 2000): 8.
89. Coate, Dan, and Keith MacDonald. "Projecting the Budget Impacts of HIPAA." Healthcare Financial Management 56, no. 2 (Feb 2002): 42-48.
90. Haugh, Rick. "Confronting HIPAA." Hospitals & Health Networks 74, no. 3 (Mar 2000): 58-62, 64.
91. Lageman, Rebecca C, and Jordan R Melick. "HIPAA: Wake-up Call for Health Care Providers." Journal of health care finance 27, no. 4 (January 2001): 1-6.
92. Rivers, Patrick A, and Kai-Li Tsai. "The Impact of the Balanced Budget Act of 1997 on Medicare in the USA: The Fallout Continues." International journal of health care quality assurance 15, no. 6 (Nov 2002): 249-254. https://doi.org/10.1108/09526860210442010.
93. Hersher, Betsy S. "The Role of the CIO: The Evolution Continues." Chap. 13 In Healthcare Information Management Systems: Cases, Strategies, and Solutions, edited by Marion J Ball, Charlotte A Weaver and Joan M Kiel, 161-172. New York, NY: Springer Science + Business Media, LLC, 2004.
94. Dendinger, Martha Jo. "The CHIME/HMT CIO Roundtable: Wearing Many Hats.". Health Management Technology 19, no. 10 (Sep 1998): 34-39.
95. Morrissey, John. "Big Bucks for Y2k: Survey Shows Healthcare Systems Are Budgeting Millions.". Modern Healthcare 28, no. 35 (Aug 31 1998): 68-70.
96. Morrissey, John. "Y2k: Ready or Not ... Survey: Millennium Bug Is Sapping Time and Resources, but Execs Are Glancing Beyond 2000." Modern Healthcare 29, no. 8 (Feb 1 1999): 52-54, 58-60, 64-74.
97. Wood, Grant M. "The Changing Role of the Health Care Chief Information Officer." Managed Care Interface 13, no. 9 (Sep 1 2000): 81-83.
98. Morrissey, John. "Y2K: The Budget-Eating Bug Takes Over: Survey Shows Healthcare Organizations Are Delaying Other Information System Improvements.". Modern Healthcare 29, no. 7 (Feb 1 1999): 42, 44, 46-48.
99. Gillespie, Greg. "CIOs Learn New Skills." Health Data Management 8, no. 3 (Mar 2000): 50-60.
100. Hersher, Betsy S. "The Evolution of the Chief Information Officer." Chap. Section 2, Chapter 2 In Healthcare Information Management Systems: A Practical Guide, edited by Marion J Ball, Judith V Douglas, Robert I O'Desky and James W Albright, 243-250. New York, NY: Springer Science + Buisiness Media, 1990.
101. Ball, Marion J, and Judith V Douglas. "The CIO's Key Role in Healthcare Strategic Planning". Computers in Healthcare 13, no. 5 (May 1992): 17, 19, 21.
102. Reavis, Maida. "The Role CIOs Must Play in Multihospital Strategic Planning.". Computers in Healthcare 13, no. 5 (May 1992): 26.
103. Correll, Richard A, and Brian T Malec. "The Chief Information Officer as a New Administrator." Chap. Section 2, Unit 2, Chapter 1 In Healthcare Information Management Systems: A Practical Guide, edited by Marion J Ball, Judith V Douglas, Robert I O'Desky and James W Albright, 235-242. New York, NY: Springer Science + Business Media, LLC, 1991.
104. Wachel, Walter. "CIO: Roles and Relationships.". Healthcare Executive 7, no. 1 (Jan/Feb 1992): 14.
105. Zinn, Tim K. "Healthcare I/S Executives Look toward the Next Decade." Computers in Healthcare 13, no. 2 (Feb 1992): 32-33,35,39.
106. Glaser, John P. "The Role of the Chief Information Officer in the Health Care Organization in the 1990s." Topics in Health Information Management 13, no. 3 (Feb 1993): 62-68.
107. McQueen, Harry E Jr. "The Healthcare CIO's Role in Business Process Redesign.". Computers in Healthcare 14, no. 2 (Feb 1993): 24, 26, 28.
108. Diedling, Linus, and Joseph Welfeld. "The Rise of the CIO.". Hospitals & Health Networks 69, no. 3 (Feb 05 1995): 34, 36, 38.
109. Griffin, Jane. "The Modern CIO: Forging a New Role in the Managed Care Era.". Journal of Healthcare Resource Management 15, no. 4 (May 1997): 16-17, 20-21.
110. Nilson, Julie T. "How to Hire the Right CIO.". Healthcare Executive 13, no. 3 (May/Jun 1998): 8-13.
111. Watson, Sharon. "The 'Perfect' Health Care CIO.". Computerworld 32, no. 38 (Sep 21 1998): 6-11.
112. Hersher, Betsy S. "The Chief Information Officer: Past, Present, and Future." In Healthcare Information Management Systems: A Practical Guide, edited by Marion J Ball, Donald W Simborg, James W Albright and Judith V Douglas, 163-172. New York, NY: Springer New York, 1995.
113. Hersher, Betsy S, Robert L Pickton, David A Weiss, and S Gardner Wright. "The CIO's Position in Today's Emerging Health Care System: Lessons Learned." Healthcare Information Management: Journal of the Healthcare Information and Management Systems Society of the American Hospital Association 10, no. 4 (Jan 1996): 21-45.
114. Lundberg, Abbie. "The Power of Cooperative Thinking." CIO Magazine (Oct 15 1997): 34-40.
115. Shapiro, Joe. Guide to Effective Healthcare Information & Management Systems and the Role of the Chief Information Officer. 3rd ed.: Healthcare Information and Management Systems Society, Jan 15, 1998.
116. Longshore, George F. "CIO Takes on Larger Role, Even at Smaller Hospitals.". Health Care Strategic Management 10, no. 11 (Nov 1992): 10, 12.
117. Hard, Rob. "The Real Thing: Future Information Needs Will Require 'True'.". Hospitals 67, no. 4 (Feb 20 1993): 36.
118. Friel, Donald F. "Enhancing It Executive Influence.". Healthcare Informatics 14, no. 4 (Apr 1997): 94, 96, 98.
119. Briggs, Bill. "CIOs Double as Change Agents.". Health Data Management 10, no. 3 (Mar 2002): 40-44.
120. Morrissey, John. "Are CIOs up to the Challenge? Survey of CEOs Finds Lack of Confidence in Info Chiefs." Modern Healthcare 27, no. 18 (1997): 19.
121. Omnibus Budget Reconciliation Act of 1989. Pub. L. No. 101-239, 1421 Stat. 1989.
122. The Data Standards Working Group. Connecting for Health: A Public-Private Collaborative. Markel Foundation (New York, NY: Markel Foundation, Jun 5 2003).
123. Medicare Prescription Drug, Improvement, and Modernization Act. Pub. L. No. 108-173, 1305 et seq, 117 Stat. 2003.
124. Bell, Douglas S, and Maria A Friedman. "E-Prescribing and the Medicare Modernization Act of 2003." Health Affairs 24, no. 5 (Sep / Oct 2005): 1159-1169. https://doi.org/10.1377/hlthaff.24.5.1159.
125. "Executive Order 13335 of April 30, 2003, Incentives for the Use of Health Information Technology and Establishing the Position of the National Health Information Technology Coordinator." Federal Register 69, no. 84 (April 30, 2004 2004): 24059-24061.
126. Shortliffe, Edward H. "Strategic Action in Health Information Technology: Why the Obvious Has Taken So Long." Health Affairs 24, no. 5 (Sep/Oct 2005): 1222-1233.
127. Kolodner, Robert M, Simon P Cohn, and Charles P Friedman. "Health Information Technology: Strategic Initiatives, Real Progress: There Is Nothing “Magical” About the Strategic Thinking Behind Health It Adoption in the United States." Health Affairs 27, no. Supplement 1 (Aug 19 2008): w391-w395. https://doi.org/10.1377/hlthaff.27.5.w391.
128. U.S. Department of Health and Human Services, Office of the National Coordinator for Health Information Technology. The Onc-Coordinated Federal Health It Strategic Plan: 2008-2012. Washington, DC: U.S. Department of Health and Human Services, 2008.
129. Health Information Technology for Economic and Clinical Health Act. Pub. L. No. 111-5, 13001 et seq, 123 Stat. 2009.
130. Jones, Charles M. "The Nature of a Successful CIO: Thriving Leaders Have Certain Characteristics, and So Do Their Organizations.". Healthcare Informatics 20, no. 10 (Oct 2003): 44-46.
131. Hagland, Mark. "The Many Hats of a CIO." Healthcare Informatics 17, no. 5 (May 2000): 69-72, 74, 76.
132. "The Healthcare CIO: C. Martin Harris, M.D., Mba, Chief Information Officer, Cleveland Clinic.". Health Management Technology 29, no. 7 (Jul 2008): 10.
133. Friel, Donald F. "The CIO as Business Futurist." Journal of Healthcare Information Management: JHIM 16, no. 4 (Fall 2002): 12-14.
134. "The Healthcare Cio: Edith Dees, VP/CIO, Holy Spirit Health System." Health Management Technology 29, no. 12 (Dec 2008): 10-11.
135. "Cio Values: Richard Temple, VP of IT and CIO, Saint Clare's Health System.". Informationweek, no. 1169 (Jan 21 2008): 14.
136. Fleming, George. "The Evolving Role of the Hospital CIO.". Health Management Technology 29, no. 7 (Jul 2008): 39-40.
137. Hagland, Mark. "The Art of the Project: Healthcare CIOs under Pressure to Manage Growing Complex Portfolios." Healthcare informatics: the business magazine for information and communication systems 25, no. 4 (Apr 2008): 48-53.
138. Schuerenberg, Beckie Kelly. "So You Want to Be a CIO?". Health Data Management 16, no. 3 (Mar 2008): 34, 36, 38 passim.
139. Glaser, John, and Judy Kirby. "Evolution of the Healthcare CIO." Healthcare Financial Management 63, no. 11 (2009): 38-41.
140. Patient Protection and Affordable Care Act. Pub. L. No. 111-148, 18001 et seq, 124 Stat. 2010.
141. Health Care and Education Reconciliation Act of 2010. Pub. L. No. 111-152, 1305 et seq, 124 Stat. 2010.
142. Blumenthal, David. "Implementation of the Federal Health Information Technology Initiative." The New England journal of medicine 365, no. 25 (2011): 2426-2431. https://doi.org/10.1056/NEJMsr1112158.
143. Centers for Medicare & Medicaid Services. Medicare & Medicaid Ehr Incentive Program. Baltimore, MD: Centers for Medicare & Medicaid Services,, 2010.
144. Wilson, Linda. "The Rise of the CMIO.". Health Data Management 23, no. 9 (Nov 2015): 12-15.
145. Kearns, Michelle. "Developing the Role of CIO in Healthcare Management: From "the IT Guy" to CIO." HealthManagement.org 17, no. 1 (Feb 17 2017): 16-17.
146. McKinney, Maureen. "CMIOs Steadily on the Rise." Article. Hospitals & Health Networks 84, no. 3 (Mar 2010): 41-42.
147. Leventhal, Rajiv. "The Evolving Healthcare CIO: Innovation over Information." Healthcare Informatics (Nov 15 2018): 11.
148. Sridharan, Shankar, Ward Priestman, and Neil J Sebire. "Chief Information Officer Team Evolution in University Hospitals: Interaction of the Three 'C's (CIO, CCIO, CRIO)." BMJ health & care informatics 25, no. 2 (2018): 88-91. https://doi.org/10.14236/jhi.v25i2.997.
149. Aitken, Murray. "Why Life Sciences Companies Need to Tap Technology to Gain a Competitive Edge—and What That Means for the Chief Information Officers (CIO) Role." Mhealth 2, no. 10 (Mar 23 2016): 1-3. https://doi.org/10.21037/mhealth.2016.03.03.
150. Sullivan, Tom, and Mike Miliard. "Meet the Modern Healthcare CIO: A Business Leader That Is Casting Off Their Traditional It Role." Healthcare IT News (Mar 29 2018).
151. Looney, William. "Transforming Technology the Future of the CIO in the Life Sciences.". Pharmaceutical Executive 36, no. 7 (Jul 2016): 16-18,20,22-27.
152. U.S. Department of Health and Human Services. "Secretary Azar Declares Public Health Emergency for United States for 2019 Novel Coronavirus." news release, January 31, 2020, https://www.hhs.gov/about/news/2020/01/31/secretary-azar-declares-public-health-emergency-us-2019-novel-coronavirus.html.
153. Centers for Disease Control and Prevention. "CDC Confirms Person-to-Person Spread of New Coronavirus in the United States." news release, January 30, 2020, https://www.cdc.gov/media/releases/2020/p0130-coronavirus-spread.html.
154. Coronavirus Aid, Relief, and Economic Security Act. Pub. L. No. 116-136, 9001 et seq, Stat. 2020.
155. Williamson, Kelley. "Online Training, Stat.". Talent Development 74, no. 8 (Aug 2020): 50-53.
156. Berry, Kathryn. "Digital, Operations, and Innovation: The Evolving Roles, Responsibilities of the Healthcare CIO." This Week Health. (Jun 8 2021). https://thisweekhealth.com/digital-operations-and-innovation-the-evolving-roles-and-responsibilities-of-the-cio/.
157. Cousins, Karlene, Attila J. Hertelendy, Min Chen, Polina Durneva, and Shangjun Wang. "Building Resilient Hospital Information Technology Services through Organizational Learning: Lessons in CIO Leadership During an International Systemic Crisis in the United States and Abu Dhabi, United Arab Emirates." International Journal of Medical Informatics 176 (2023/08/01/ 2023): 105113. https://doi.org/10.1016/j.ijmedinf.2023.105113.
158. Butcher, Lola. "The Rise of the Healthcare CIO.". Physician Leadership Journal 8, no. 3 (May/Jun 2021): 20-22.
159. Upton, Julian. "Defining the Chief Data Officer.". Pharmaceutical Executive 41, no. 10 (Oct 2021): 26-28.
Figure 1 – Search Process
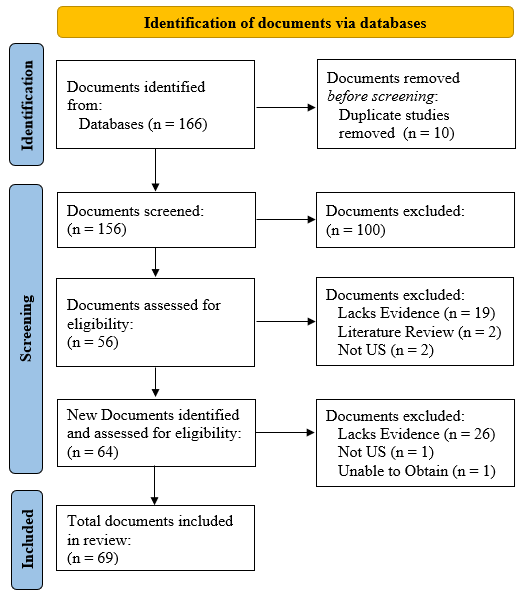
Table 1 – HIS Executives Roles, Responsibilities, and Attributes
Author Biographies
Douglas A. Jones, MBA, MSHA, (djone@uab.edu) is a PhD student at the University of Alabama at Birmingham and an Assistant Professor in the Master’s of Health Administration Program at Auburn University at Montgomery.
Nancy Borkowski, DBA, CPA, FACHE, FHFMA, is a Distinguished Professor in the Department of Health Services Administration at the University of Alabama at Birmingham.
Christy Harris Lemak, PhD, is Professor of Health Services Administration at the University of Alabama at Birmingham where she teaches and conducts research on high performance in health care and leadership’s contribution to accelerating the digital transformation of the US health system.
Dae Hyun (Daniel) Kim, PhD, is an Assistant Professor of Health Management and Policy at Georgetown University's School of Health. His research portfolio centers around quality improvement with a focus on health literacy, well-being, and education, with the aim of bridging gaps within the context of healthcare organizations.
Dalton E. Pena, MSHA, is a PhD student and graduate research assistant at the University of Alabama at Birmingham. His research is focused on the role of the CIO, the CIO / CEO relationship, and the role of CIO in accelerating organizational transformation.